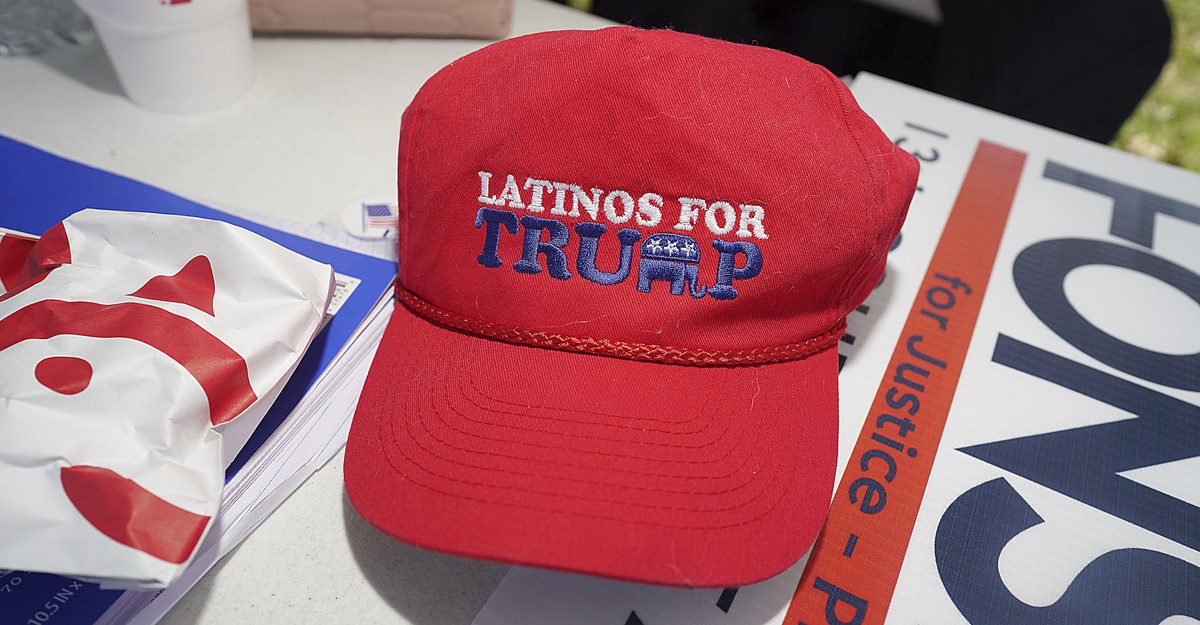
Judith Dambowic, a a number of myeloma affected person, on her porch in Oakland, CA, proper earlier than shaving her head in preparation for a stem cell transplant in Might. Dambowic needed California to move a regulation regulating Medigap insurance coverage insurance policies. The reform, which finally failed, would have made it simpler for her to modify her protection from Medicare Benefit to conventional Medicare.
Judith Dambowic
conceal caption
toggle caption
Judith Dambowic
Many seniors are grateful once they flip 65 and grow to be eligible for Medicare. However to get enrolled they first must make an enormous choice — selecting a Medicare plan.
The preliminary alternative is whether or not to go together with conventional Medicare or Medicare Benefit.
Conventional Medicare has deductibles, co-pays, and co-insurance, and the additional prices can add up. To fill within the gaps, individuals usually purchase a non-public supplemental plan, referred to as Medigap insurance coverage.
“One of many most important advantages of Medigap is that it offers individuals on Medicare predictable bills, as a result of individuals pay month-to-month premiums to keep away from unpredictable bills in the event that they get sick,” stated Tricia Neuman, Government Director for KFF’s Program on Medicare Coverage.
This mix additionally provides individuals probably the most choices in selecting docs, as a result of most settle for conventional Medicare.
The opposite choice a newly-eligible senior can select is Medicare Benefit. This plan, bought by a non-public insurance coverage firm, streamlines the upfront prices, making a separate Medigap plan pointless.
Insurance coverage corporations usually closely market their Medicare Benefit plans, and supply further advantages like dental and imaginative and prescient insurance coverage.
Due to the preliminary enchantment of Medicare Benefit plans, over half of individuals eligible for Medicare opted for a Medicare Benefit plan in 2023.
However there’s a serious downside to Medicare Benefit plans: they lock sufferers right into a most popular community of docs and hospitals, narrowing choices for remedy.
“They may be, 65, 66, 67 — within the scheme of issues, they’re at their healthiest, nevertheless it might be that over the course of a number of years, they develop a critical sickness,” stated Neuman.
The restricted nature of the Benefit plans, Neuman added, means seniors won’t be capable of go to the specialists they need.
Generally seniors resolve they’d fairly have the pliability and selection of suppliers out there below conventional Medicare, and attempt to change again.
However they may be caught. In the event that they attempt to change again after the primary 6 months of enrollment in Medicare, there’s no assure they’ll get a Medigap coverage to pair with conventional Medicare.
That’s as a result of non-public insurers who problem Medigap insurance policies have the ability to refuse protection or set a excessive worth, as soon as the six-month window is closed.
“Folks could be denied a coverage as a result of they’ve a pre-existing situation, or they are often charged extra, or they’ll get the coverage — however not for the actual situation that can require medical consideration,” Neuman stated.
These protection denials and worth hikes had been frequent within the particular person medical health insurance market earlier than reforms below the Inexpensive Care Act. However the ACA’s rules don’t apply to seniors in search of Medigap plans after the six-month window.
California takes a stab at opening Medigap enrollment
A invoice that might have modified that was launched within the California legislature this 12 months.
Driving the trouble was concern amongst legislators that California seniors on Medicare Benefit plans had been going through fewer and fewer selections of their networks.
In 2023, Scripps Well being, a serious San Diego hospital system, stopped accepting Medicare Benefit plans, saying the plans paid lower than different insurers for a similar therapies, and required docs to navigate prior authorization protocols that had been burdensome and time-consuming.
The transfer despatched seniors within the San Diego area scrambling to enroll in conventional Medicare, supplemented by Medigap plans. The excessive numbers of people that discovered Medigap plans unaffordable drew the eye of State Senator Catherine Blakespear, who put ahead a Medigap reform invoice.
4 states reformed Medigap within the Nineties — Connecticut, Maine, Massachusetts, and New York. The remaining, together with California, enable Medigap insurers vast leeway in setting costs and issuing denials.
California’s invoice would have created a 90-day open enrollment interval for Medigap, each single 12 months. That might enable seniors to opt-in or out every year and never be denied — or face exorbitant premiums attributable to pre-existing situations.

Insurance coverage trade consultant Steffanie Watkins testifies April 24 earlier than the Senate Standing Committee on Well being, in opposition to a invoice that might have created an annual open enrollment interval for Medigap insurance coverage. This might have allowed seniors higher flexibility in switching from Medicare Benefit plans to conventional Medicare.
Senate of the State of California
conceal caption
toggle caption
Senate of the State of California
The Leukemia and Lymphoma Society turned a serious supporter of the trouble to move the invoice.
“Most cancers or any persistent sickness could be very, very costly, and that is why having supplemental protection is vital,” stated Adam Zarrin, a coverage analyst for the Society. “The second half is about ensuring that sufferers have entry to the very best well being care out there.”
Zarrin says leukemia and different blood cancers are extra generally identified in older adults, after age 55.
That was the case for Oakland resident Judith Dambowic.
Dambowic was 58 and dealing as a bodily therapist when she discovered her swollen and painful eye was a symptom of a number of myeloma, a most cancers of the bone marrow.
Ten years after being identified, Dambowic has grow to be a affected person advocate within the effort to reform Medigap in California.
“It is the choices. It is the selection that issues,” she stated.
Dambowic has a Medicare Benefit plan, and for the second, she is happy along with her community selections. However along with her most cancers, conventional remedy choices usually cease working to handle the illness.
Dambowic needs flexibility sooner or later to hunt out completely different clinicians, and even experimental trials.
“These slots are extremely coveted and it is very onerous to get in from an Benefit plan. And the Benefit plans aren’t actually working these leading edge medical trials,” Dambowic stated.
However until the rules change, Dambowic must keep in Medicare Benefit. She thinks it’s unlikely she might get a Medigap coverage that might enable her to return to conventional Medicare.
There’s some proof that signifies most cancers sufferers might have fewer choices in Medicare Benefit.
A current examine within the Journal of Medical Oncology discovered “[Medicare Advantage] beneficiaries have important obstacles in accessing optimum surgical most cancers care,” when in comparison with individuals with conventional Medicare.
Insurance coverage charges would enhance, trade fights again
Because the invoice was being debated within the state Capitol this spring, Steffanie Watkins spoke to lawmakers on behalf of the insurance coverage foyer.
If extra sick Californians are capable of transfer onto Medigap plans, Watkins argued, insurance coverage corporations must elevate premiums for everybody.
“We’re involved with the potential devastating impacts this invoice might have on the 1.1 million seniors who, by no fault of their very own, would expertise important charge will increase if this invoice had been to move,” she stated.
A state finances evaluation of the proposed invoice discovered the typical Medigap premium would enhance by 33 p.c, about 80 {dollars} a month.
That’s a legitimate concern, in keeping with KFF’s Tricia Neuman.
“For individuals with modest incomes, individuals [on]of the type of decrease finish of the revenue scale who’ve Medigap, they may really feel priced out of the market,” she stated.
Ultimately, the invoice didn’t make it out of the appropriations committee to advance to a full vote within the Senate.
Zarrin blamed legislators for siding with the insurance coverage corporations, however stated his group will maintain pushing for this reform in future periods.
Judith Dambowic was additionally disillusioned.
For now, she’ll proceed to deal with educating buddies and different most cancers sufferers about their Medicare choices, in order that they know what they’re signing up for from the beginning — and the way tough it may be to vary.
This story comes from NPR’s well being reporting partnership with CapRadio and KFF Well being Information.

:max_bytes(150000):strip_icc()/blakelivelyfb-5480101bb936454ab729b34f1921a019.jpg)