This text was initially printed by Knowable Journal.
Peering by means of his microscope in 1910, the Franco-Canadian microbiologist Félix d’Hérelle seen some “clear spots” in his bacterial cultures, an anomaly that turned out to be viruses preying on the micro organism. Years later, d’Hérelle would come to make use of these viruses, which he known as bacteriophages, to deal with sufferers plagued with dysentery after World Conflict I.
Within the a long time that adopted, d’Hérelle and others used this phage remedy to deal with bubonic plague and cholera, till the method fell into disuse after the widespread adoption of antibiotics within the Forties.
However now, with micro organism evolving resistance to increasingly more antibiotics, phage remedy is drawing a re-assessment from researchers—typically with a novel twist. As an alternative of merely utilizing the phages to kill micro organism straight, the brand new technique goals to catch the micro organism in an evolutionary dilemma, one during which they can’t evade phages and antibiotics concurrently.
This plan, which makes use of a way known as “phage steering,” has proven promising leads to preliminary exams, however the scope of its usefulness stays to be confirmed.
There’s definitely a necessity to search out new methods to answer bacterial infections. Greater than 70 % of hospital-acquired bacterial infections in america are immune to a minimum of one kind of antibiotic. And a few pathogens, reminiscent of Acinetobacter, Pseudomonas, Escherichia coli, and Klebsiella—categorized by the World Well being Group as among the greatest threats to human well being—are immune to a number of antibiotics. In 2019, antimicrobial resistance was linked to 4.95 million deaths globally, heightening the decision for simpler remedy choices.
One of many ways in which micro organism can evolve resistance to antibiotics is through the use of buildings of their membranes which might be designed to maneuver undesirable molecules out of the cell. By modifying these “efflux pumps” to acknowledge the antibiotic, micro organism can eradicate the drug earlier than it poisons them.
Because it seems, some phages seem to make use of these similar efflux pumps to invade the bacterial cell. The phage presumably attaches its tail to the outer portion of the pump protein, like a key slipping right into a lock, after which injects its genetic materials into the cell. This fortunate coincidence led Paul Turner, an evolutionary biologist at Yale College, to recommend that treating a affected person with phages and antibiotics concurrently may entice micro organism in a no-win state of affairs: In the event that they evolve to switch their efflux pumps so the phage can’t bind, the pumps will not expel antibiotics, and the micro organism will lose their resistance. But when they preserve their antibiotic resistance, the phages will kill them, as Turner and colleagues defined within the 2023 Annual Evaluation of Virology.
The outcome, in different phrases, is a two-pronged assault, says Michael Hochberg, an evolutionary biologist on the French Nationwide Centre for Scientific Analysis who research the right way to stop the evolution of bacterial resistance: “It’s sort of like a crisscross impact.” The identical precept can goal different bacterial molecules that play a twin position in resistance to viruses and antibiotics.
Turner examined this speculation on the multidrug-resistant Pseudomonas aeruginosa, which causes harmful infections, particularly in health-care settings. This bacterium has 4 efflux pumps concerned in antibiotic resistance, and Turner predicted that if he may discover a phage that used one of many pumps as a method into the cell, the bacterium can be compelled to slam the door on the phage by mutating the receptor—thereby impeding its potential to pump out antibiotics.
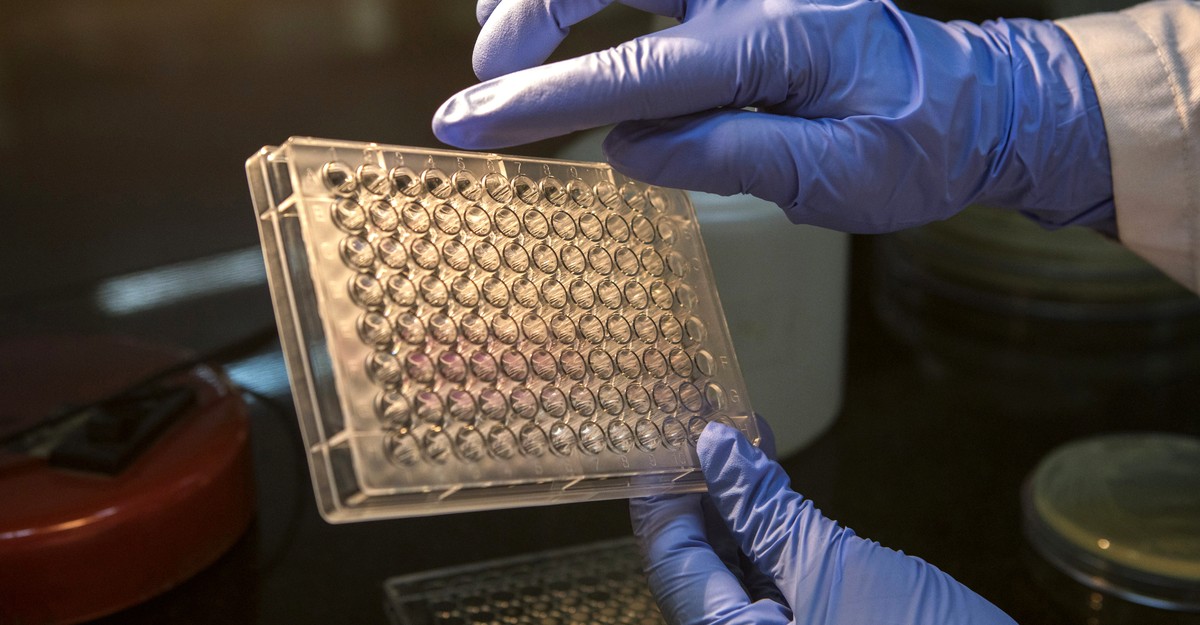
Sampling from the setting, Turner’s staff collected 42 phage isolates that infect P. aeruginosa. Out of all of the phages, one, OMKO1, sure to an efflux pump, making it the proper candidate for the experiment.
The researchers then cultured antibiotic-resistant P. aeruginosa along with OMKO1, hoping this may power the bacterium to switch its efflux pump to withstand the phage. They uncovered these phage-resistant micro organism, in addition to their regular, phage-sensitive counterparts, to 4 antibiotics the micro organism had been immune to: tetracycline, erythromycin, ciprofloxacin, and ceftazidime.
As the idea predicted, the micro organism that had developed resistance to the phage have been extra delicate to the antibiotics than people who had not been uncovered to the phage. This implies that the micro organism had, certainly, been compelled to lose their antibiotic resistance by means of their have to struggle off the phage.
Different researchers have additionally proven that phage steering can resensitize micro organism to widespread antibiotics they’d turn out to be immune to. One examine, by a world analysis staff, confirmed {that a} phage known as Phab24 can be utilized to restore sensitivity to the antibiotic colistin in Acinetobacter baumannii, which causes life-threatening ailments.
In a second examine, researchers at Monash College, in Australia, sampled infectious micro organism from sufferers. They discovered A. baumannii micro organism uncovered to the phages ΦFG02 and ΦCO01 had inactivated a gene that helps create the microbe’s essential outer layer, or capsule. This layer serves because the entry level for the phages, however it additionally helps the bacterium type biofilms that maintain out antibiotics—so eradicating the layer rendered A. baumannii vulnerable to a number of antibiotics that it was beforehand immune to.
In a 3rd examine, researchers in England found that when a P. aeruginosa pressure that was immune to all antibiotics was uncovered to phages, the bacterium turned delicate to 2 antibiotics that have been in any other case thought of ineffective towards P. aeruginosa.
Turner’s staff has used phage steering in dozens of circumstances of customized remedy in scientific settings, says Benjamin Chan, a microbiologist at Yale College who works with Turner. The outcomes, many nonetheless unpublished, have been promising thus far, Chan says. Nonrespiratory infections are comparatively straightforward to clear off, and lung infections, which the phage-steering strategy wouldn’t be anticipated to eradicate fully, typically present some enchancment. “I’d say that we have now been fairly profitable in utilizing phage steering to deal with difficult-to-manage infections, lowering antimicrobial resistance in lots of circumstances,” he says. However he notes that it’s typically tough to find out whether or not phage steering actually was answerable for the cures.
Phage remedy could not work for all antibiotic-resistant micro organism, says the molecular biologist Graham Hatfull of the College of Pittsburgh. That’s as a result of phages are very host-specific, and for many phages, nobody is aware of what goal they bind to on the bacterial cell floor. For phage steering to work towards antibiotic resistance, the phage has to bind to a molecule that’s concerned in that resistance—and it’s not clear how typically that fortuitous coincidence happens.
Jason Gill, who research bacteriophage biology at Texas A&M College, says that it’s not straightforward to foretell if a phage will induce antibiotic sensitivity. So you must hunt for the appropriate virus every time.
Gill is aware of from expertise how difficult the strategy can get. He was a part of a staff of researchers and medical doctors who used phages to deal with a affected person with a multidrug-resistant A. baumannii an infection. Lower than 4 days after the staff administered phages intravenously and thru the pores and skin, the affected person awakened from a coma and have become attentive to the beforehand ineffective antibiotic minocycline—a putting success.
However when Gill tried an analogous experiment in cell cultures, he acquired a distinct outcome. The A. baumannii developed resistance to the phages, however additionally they maintained their resistance to minocycline. “There’s not an entire mechanistic understanding,” Gill says. “The linkage between phage resistance and antibiotic sensitivity in all probability varies by bacterial pressure, phage, and antibiotic.” Meaning phage steering could not all the time work, he says.
Turner, for his half, factors out one other potential drawback: that phages may work too effectively. If phage remedy kills giant quantities of micro organism and deposits their stays within the bloodstream shortly, for instance, this might set off septic shock in sufferers. Scientists haven’t fairly found out the right way to tackle this drawback.
One other concern is that medical doctors have much less exact management over phages than over antibiotics. “Phages can mutate; they will adapt; they’ve a genome,” Hochberg says. Security considerations, he notes, are one issue inhibiting the routine use of phage remedy in international locations reminiscent of america, limiting it to case-by-case functions reminiscent of Turner and Chan’s.
Phage remedy could have been too high-tech for the Forties, and even in the present day, scientists wrestle with the right way to use it. What we want now, Turner says, are rigorous experiments that may train us the right way to make it work.

:max_bytes(150000):strip_icc()/3-ffeed5c76dfe421fbee3829abd564958-08e5d462de124ba996bc51b6f8c3147a.jpg)